In this video Professor Anne Phillips and Co-Chair of iDEAL Diabetes CIC introduces about diabetes and living with skin condition with diabetes and discusses the value to the resources within this webpage regarding increasing knowledge and awareness about various skin conditions related to living with diabetes.
This animation which can be viewed below offers you opportunity to promote LET’S SUPPORT NOW and encourages its use with every person with diabetes
(Click the image below to play video)
–
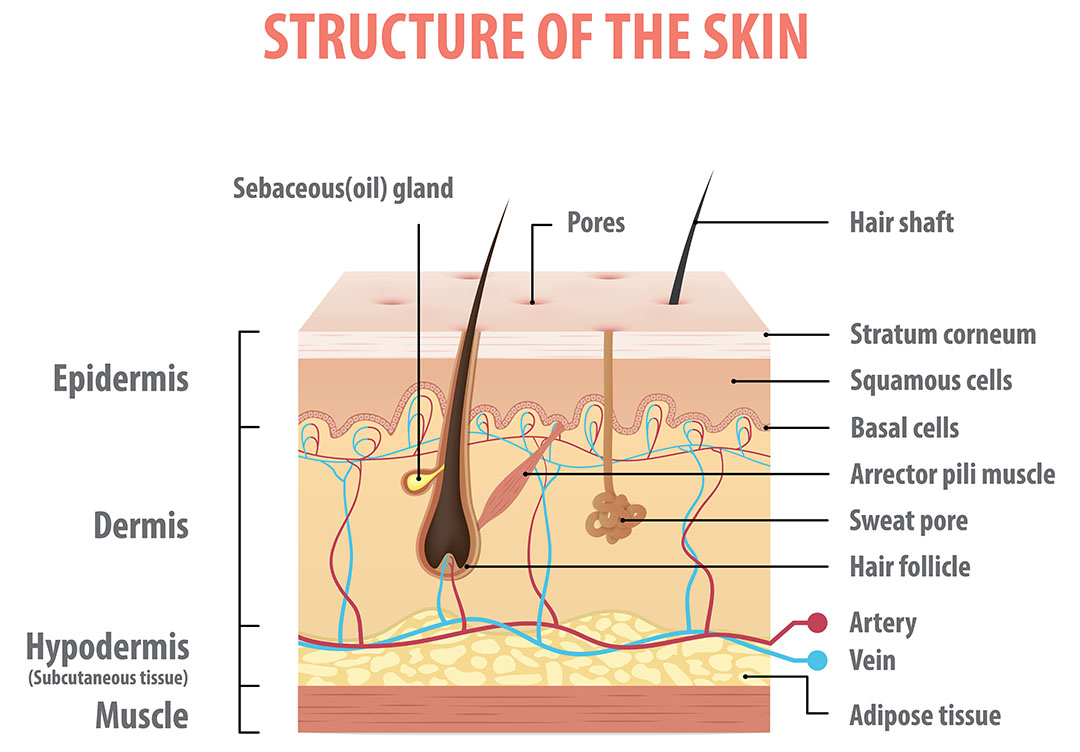
The skin is part of the integumentary system, which also includes hair and fingernails, and it is the largest organ of the human body. A skin problems are often the first sign that a person has diabetes.
Diabetes affects various parts of your body, including your skin. An estimated 1 in 3 people with diabetes (Type 1 or Type 2) will develop a skin rash or other skin problem at some point. Diabetes mellitus is a common and debilitating disease that affects a variety of organs including the skin. A variety of dermatologic manifestations have been linked with diabetes mellitus; these conditions vary in severity and can be benign, deforming, and even life-threatening. Such skin changes can offer insight into individuals glycaemic control and may be the first sign of metabolic derangement in people not yet diagnosed with diabetes. Recognition and management of these conditions is important in maximizing the quality of life and in avoiding serious adverse effects in people with diabetes mellitus.
This webpage gives practitioners an indication of what to look out for when working in partnership with people with diabetes.

–
Diabetes can affect every part of the body and it increasingly presents with skin complications. Suboptimal glycaemic control affects the glycosylation of proteins, lipids and other organic molecules, which can have a profound effect on the structure of proteins in the skin and cause skin manifestations. As a result, the skin’s integrity and its ability to repair damage and resist infection can be compromised.
Overall prevalence of cutaneous disorders does not seem to differ between people with type 1 or type 2 diabetes but people with type 1 diabetes appear to develop more autoimmune-type cutaneous lesions whereas people with type 2 diabetes tend to develop more frequent skin infections. People with type 2 diabetes are also prone to developing more insulin resistance-type lesions. Fortunately, if recognised and diagnosed early, most skin conditions can be prevented or treated. While some skin problems can affect anyone (such as impetigo or psoriasis), people with diabetes tend to get skin complications such as bacterial infections, fungal infections and pruritis more easily.

Good skin care
There are several things people with diabetes can do to prevent skin problems:
- Keep diabetes well managed. People with high glucose levels tend to have dry skin and less ability to fend off harmful bacteria. Both conditions increase the risk of infection.
- Keep skin clean and dry.
- Avoid very hot baths and showers. If the skin is dry, don’t use bubble baths. Moisturizing soaps may help. Afterward, use a standard skin lotion, but don’t put lotions between toes. The extra moisture there can encourage fungus to grow.
- Prevent dry skin. Scratching dry or itchy skin can open it up and allow infection to set in. Moisturize the skin to prevent chapping, especially in cold or windy weather.
- Treat cuts right away. Wash minor cuts with soap and water. Only use an antibiotic cream or ointment if your doctor says it’s okay. Cover minor cuts with sterile gauze. See a doctor right away if you get a major cut, burn, or infection.
- See a dermatologist (skin doctor) about skin problems if the person with diabetes is not able to solve them themselves.
- Talk to a health care professional if the individual is not able to solve a skin problem themselves.
- Take good care of your feet. Check them every day for sores and cuts. Wear broad, flat shoes that fit well. Check your shoes for foreign objects before putting them on.
This link takes you to the ACT NOW webpage resources about foot health and when to seek help with foot problems and diabetes:
–
Other skin problems can affect people with diabetes and people at risk of diabetes with non-diabetic hyperglycaemia, these include:
Please click on each section for more information
Diabetes can be associated with pruritus, more often localised than generalised. Hyperglycaemia can also make people experiencing itchy skin also. Pruritus or itchy skin is more likely in people with diabetes who also have dry skin or neuropathy. Specifically for people with type 2 diabetes primary risk factors are identified as age, duration of diabetes, diabetes related peripheral neuropathy, retinopathy, chronic kidney disease and raised fasting plasma glucose levels. Moisturizing the area affected by cooled fragrance free body lotions can help reduce the itching and rehydrate the skin also.
Xerosis is one of the most common skin presentations in people with diabetes and has been reported to be present in as many as 40% of people with diabetes. Xerosis refers to skin that is abnormally dry. Affected skin may present with scaling, cracks, or a rough texture. These skin changes are most frequently located on the feet of people with diabetes. It has been reported that people with diabetes who also have obesity will experience more severe hypohidrosis of the feet. In people with diabetes, xerosis occurs often in the context of microvascular complications To avoid complications such as fissures and secondary infections, xerosis can be managed with emollients.

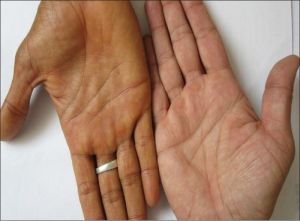
Acanthosis nigricans is a classic dermatologic manifestation of diabetes mellitus that affects men and women of all ages. This occurs more commonly in type 2 diabetes and is more prevalent in those with darker-skin colour. This condition is observed in a variety of endocrinopathies associated with resistance to insulin such as acromegaly, Cushing syndrome, obesity, polycystic ovarian syndrome, and thyroid dysfunction.
Acanthosis Nigricans presents chronically as multiple poorly demarcated plaques with grey to dark-brown hyperpigmentation and a thickened velvety to verrucous texture. Classically, it has a symmetrical distribution and is located in intertriginous or flexural surfaces such as the back of the neck, axilla, elbows, palmer hands (also known as “tripe palms”), inframammary creases, umbilicus, or groin. Affected areas are asymptomatic; however, extensive involvement may cause discomfort or can smell.
Acanthosis Nigricans should prompt evaluation for diabetes mellitus and for other signs of insulin resistance.

Images from NHS
TREATMENT
Treatment of Acanthosis Nigricans may improve current lesions and prevent future cutaneous manifestations. It is best managed with lifestyle changes such as dietary modifications, increased physical activity, and weight reduction. In people with diabetes, pharmacologic treatments such as metformin, that improve glycaemic control and reduce insulin resistance are also beneficial. Primary dermatologic therapies are usually ineffective especially in people with generalized involvement. However, in those with thickened or macerated areas of skin, oral retinoids or topical keratolytics such as ammonium lactate, retinoic acid, or salicylic acid can be used to alleviate symptoms.
–
Infections
Diabetes presents a significant risk factor for all kinds of infections. The infections are more likely to be frequent and can have a poorer response to treatments. Hyperglycaemia can occur as a result of infection and guidance regarding sick Day Advice is vital to help reduce hyperglycaemia to help improve and cure infections. Insulin and also metformin can help immune function. Bacterial infections do need antibiotic therapy prescribed.
Skin and soft Tissue Infections can present as the following:
Please click on each section for more information
This is the most common skin and soft tissue infection seen in people with diabetes. The most common organism is Staph species.
For abscess culture is needed and incision and drainage is required. Oral antibiotics are also required.

A skin abscess looks like a raised, painful lump. It’s typically 1–3cm across, though it can get much larger. It also has a pocket, or collection, of pus under the skin. It may or may not drain or leak on its own. Abscesses can also occur anywhere on the body, but they’re most likely to affect the groin, buttocks, armpits, back or limbs.

Cellulitis can affect any part of the body, but it most often affects the legs. It usually starts as a small patch but can spread to cover large areas. With cellulitis, the person may also have a fever, chills, and fatigue.
Styes (infections of the glands of the eyelid)

Boils

Folliculitis (infections of the hair follicles)

Panroychia (Infections around the nails)

–
Fungal

Itching or pruritus of the genitalia or in skin areas touching together can be caused by fungal infections and need to be kept clean and dry and treated with oral or cream applications of antifungal preparations. The yeast-like fungus caused by Candida albicans can create itchy rashes of moist, red areas surrounded by blisters and scales. These infections often occur in warm, moist folds of skin. Problem areas are under the breasts, around the nails, between fingers and toes, in the corners of the mouth, under the foreskin (in uncircumcised men), and in the armpits and groin. Common fungal infections include jock itch, athletes foot, ringworm (a ring-shaped itchy patch) and vaginal infections that causes itching
–
Technology related skin reactions

There have been increasing reports of skin irritation and reactions to continuous glucose monitors and insulin pumps. Skin problems are a common side effect for people using sensors and insulin pumps. At the ISPAD (International Society for Paediatric and Adolescent Diabetes) Congress 2023, the first results were shared from the SKIN-PEDIC study, which sought to identify these problems. The findings highlight the importance of awareness and proactive care to prevent and treat skin reactions.
“It’s really important when you use diabetes devices, that you are aware that you can get skin reactions, and that many actually do have certain skin problems. We as healthcare professionals need to be aware of it, and look at the skin, and also try to help them in order to intervene in the early phases of the reactions. You can prevent some of the reactions by good skin care, mainly the wounds and the skin injury. For the eczema reaction you need to often use patches underneath.” – Dr Anna Korsgaard, endocrinologist Steno Diabetes Center, Denmark, ISPAD2023
Please click here to see the advice of ISPAD https://www.diabetotech.com/blog/skin-issues-caused-by-diabetes-devices-tips-for-prevention-and-treatment
The skin problems were divided into four categories, namely:
-
skin lesions (wounds and scars)
-
eczema (contact dermatitis)
-
infection
-
lipodystrophy (lipohypertrophy or lipoatrophy)
Besides these 4 categories of skin problems, the most common complaint of people is itching.
This occurs in 23% to 77% of people who wear an insulin pump or sensor.
Itching can lead to reduced concentration at school, sleep problems, and the device loosening from scratching.
Scratching also deteriorates the skin barrier, and you are back more likely to have skin problems.
As a healthcare provider, it is therefore important to be aware of, and actively question, the high prevalence of skin problems with sensor and pump use.
Problems usually occur 4-10 months after starting the device, and the main symptoms are itching, pain and redness.
Moreover, it is essential to check the skin for lipodystrophy, as this still occurs in more than 10% of pump users. By responding in time, bigger problems can be avoided.
Please click on each section for more information
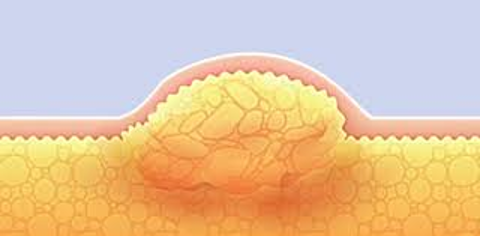
Lipohypertrophy is a fairly common condition for people with diabetes. A lump of fat and sometimes scar tissue is formed under the skin from repeated insulin injections or infusions. It occurs most often in people with diabetes who must undergo multiple daily injections, but can also occur in people who wear multiple devices such as an insulin pump and continuous glucose monitor.
Notwithstanding advancements in diabetes technology and medications, this still poses an issue because the accumulation of insulin in a particular area can result in glucose variability, including hyper and hypoglycaemia. This variability can increase insulin requirements (often unnecessarily), which implicates cost and potentially quality of life.
Lipohypertrophy presents as the most common skin complication of diabetes. Additionally, there are less obvious symptoms of lipohypertrophy, such as a change in glycaemic control.
The physical symptoms of lipohypertrophy include swollen, hard, lumpy deposits of fat and scar tissue under the skin. The skin area may also feel firmer than other areas. These areas should not be warm or painful.
Other risk factors for lipohypertrophy include:
- Repeated reuse of the same needle
- Frequency of daily injections
- Taking insulin therapy for a long time
- Improper injection technique
- Length of needle
- Hypoglycaemia
- High haemoglobin A1c
- High body mass index (BMI)


If someone with diabetes has lipohypertrophy and continues to inject insulin into the affected tissue or uses that site for an insulin pump or continuous glucose monitor, they can have erratic glycaemic due to changes in insulin absorption.
Glycaemic variability will depend on the amount and type of insulin used. For example, if someone is injecting long-acting insulin into an affected area, the insulin can remain at the site for longer periods of time, resulting in hyperglycaemia. While the insulin remains in the site, it can further enhance lipohypertrophy.
Please click on each section for more information
People with diabetes who take insulin are at an increased risk of lipohypertrophy. There are several causes that can increase the risk of lipohypertrophy, but it is most common in people who receive multiple daily injections or those who wear insulin pumps or continuous glucose monitors and do not practice proper site rotation. Increasing doses of insulin and longer duration of insulin therapy also increased the risk of lipohypertrophy.
Repeated insulin injection into the same area and inability to space injections within the same site area is the most common cause of lipohypertrophy. Sometimes people with diabetes are unaware they are even doing this, while other people prefer to inject into these areas because it doesn’t hurt as much as undamaged skin.
Needle reuse—using a needle multiple times without changing it—can also increase the risk of lipohypertrophy. In addition, people who are thinner may also be at increased risk because they have less surface area to inject insulin.4
Site lipohypertrophy can vary in size and shape—ranging from a small pea size to a tennis ball. An area of skin that has lipohypertrophy will usually be visually noticeable, though this is not always the case. In some instances, there is no lump at all and rather a harder patch of skin.
It is recommended that people who are caring for others with diabetes always check injection sites, especially if a person is noticing a change in blood sugar. Examination of injection sites through palpation and visual inspection often pinpoints the cause.
The newer insulin analogs can make these skin changes very subtle, so it is important to actually feel the area you use to inject or infuse insulin.
To assess this on your own, firmly stroke the areas in a sweeping motion to feel for any lumps. If a site is found, a healthcare provider can assist in navigating barriers as to why changing sites is problematic and educate you on proper technique.
The main treatment is to avoid the affected area and rotate sites regularly. Changing needles after each injection is also necessary.
For those people who are using pumps or continuous glucose monitors, changing sites as prescribed is recommended. If you are using the buttocks, for example, and it’s time to change your site, you should move the injection site a finger’s length (about an inch) away from the last site. You can use a chart or a calendar to help you keep track.
Aesthetically, lipohypertrophy can be unappealing, but the good news is that if it’s caught early, the skin can heal and become smoother. Adjusting to new insulin sites can also be a bit overwhelming in the beginning.
–
Diabetic dermopathy
This is a term to describe the small, round, brown atrophic skin lesions that occur on the shins of people with diabetes. This tends to occur more frequently in people who have had diabetes for at least 10-20 years and can occur more frequently in people with diabetes and also retinopathy, neuropathy and nephropathy.
In people with darker skin, the skin lesions of diabetic dermopathy can appear as very dark-coloured, slightly elevated lesions as displayed in this image.
Images sourced with permission from Diabetic Dermopathy Condition, Treatments and Pictures for Adults – Skinsight
The presence of four or more lesions is almost always limited to people with diabetes, and people presenting with shin spots not already diagnosed with diabetes are advised to undergo investigation for potential undiagnosed diabetes.
Treatment:
Diabetic dermopathy lesions or shin spots are harmless and usually do not require any treatment/ If related to suboptimal glucose control, they can disappear when glycaemic control is improved also.
–
Necrobiosis lipoidica diabeticorum
People usually present with shiny, asymptomatic patches that slowly enlarge over months – years. The patches are initially red-brown and progress to yellow, depressed atrophic plaques. Ulcerations can occur, typically following trauma and occasionally the plaques are associated with physical pain.
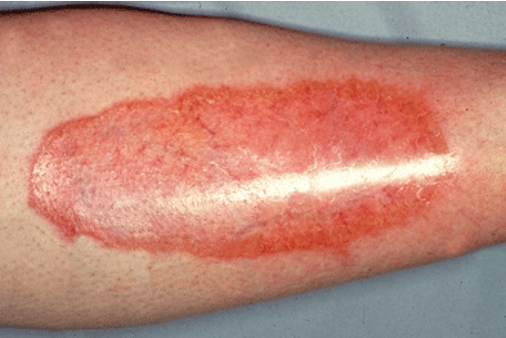

The cause of Necrobiosis lipoidica diabeticorum is unknown. It is thought to be linked to blood vessel inflammation related to autoimmune factors. This damages proteins in the skin (collagen).
People with type 1 diabetes are more likely to be affected by this condition than people with type 2. Women are more affected than men. Smoking increases the risk of this condition. Less than 0.5 of 1% of people with diabetes are affected by this skin condition.
The skin lesions start as firm, smooth, red bumps (papules) on the shins and lower part of the legs. They usually appear in the same areas on opposite sides of the body. They are painless in the early stage.
As the papules become bigger, they flatten. They develop a shiny yellow brown centre with raised red to purplish edges. Veins are visible below the yellow part of the lesions. The lesions are irregularly round or oval with well-defined borders. They can spread and join together to give the appearance of a patch.
Lesions can also occur on the forearms. Rarely, they may occur on the stomach, face, scalp, palms, and soles of the feet.
Trauma may cause the lesions to develop ulcers. Nodules also may develop. The area may become very itchy and painful.
This condition is different from ulcers that can occur on the feet or ankles in people with diabetes.
Health care professionals can examine the skin to confirm the diagnosis. If needed, a punch biopsy to diagnose the disease may be performed. The biopsy removes a sample of tissue from the edge of the lesion.
The plaques can be difficult to treat. Control of blood glucose does not improve symptoms.
- Corticosteroid creams
- Injected corticosteroids
- Drugs that suppress the immune system
- Anti-inflammatory drugs
- Medicines that improve blood flow
- Hyperbaric oxygen therapy may be used to increase the amount of oxygen in the blood to promote healing of ulcers
- Phototherapy, a medical procedure in which the skin is carefully exposed to ultraviolet light
- Laser therapy
In severe cases, the lesion may be removed by surgery, followed by moving (grafting) skin from other parts of body to the operated area.
Avoid injury to the area to prevent the lesions from turning into ulcers.
Smoking can slow healing of the lesions.
Outlook (Prognosis)
NLD is a long-term disease. Lesions do not heal well and can recur. Ulcers are difficult to treat. The appearance of the skin may take a long time to become normal, even after treatment. People affected can be psychologically distressed as this condition is such a visual reminder of their diabetes. Careful counselling and use of language that matters is pivotal when caring for people with this and any other skin condition.
–
Bullosis diabeticorum (diabetic blisters)
Bullous diabeticorum is a rare cutaneous manifestation of diabetes. It is frequently underdiagnosed, misdiagnosed and not treated properly. The blisters can appear spontaneously and the majority of people affected have pre-existing complications such as nephropathy and neuropathy. This condition is twice as common in males with diabetes.
The blisters are painless, tense blisters arising from non-inflamed skin. Spontaneous bullae may be the first sign of underlying glycaemic control. Blisters appear in varying sizes measuring 0.5 – 17cm diameter, containing sterile fluid. Onset is abrupt and can develop overnight. The blisters are usually painless but some people can report discomfort or a burning sensation. The blisters appear more frequently on lower limbs, especially the tips of toes and plantar surfaces of the feet.
Images from Cleveland Clinical Journal of Medicine
The risk of further infection is the most critical concern therefore a prompt level of awareness is required. This is a self-limiting condition and usually resolves spontaneously within 2-6 weeks without scarring.
–
Diabetic thick skin known as Scleredema diabeticorum


Finger pebbles in someone with diabetes (Images from Wiley online)


Skin thickening is frequently seen in people with diabetes. Affected areas of skin can appear thickened, waxy or oedematous. People affected are often asymptomatic but can have a reduction in sensation and pain. Although different parts of the body can be affected, the hands and feet are the most frequently involved. The back of the neck, shoulders, upper arms and upper back can also be affected.
Huntley’s papules, also known as finger pebbles, are a benign cutaneous finding affecting the hands. People present with clusters of non-erythematous, asymptomatic, small papules on the dorsal surface of the hand, specifically affecting the metacarpophalangeal joints and periungual areas. The clusters of small papules can develop into coalescent plaques. Other associated cutaneous findings include hypopigmentation and induration of the skin. Huntley’s papules are strongly associated with type 2 diabetes and may be an early sign of diabetic thick skin. Topical therapies are usually ineffective; however, people experiencing from excessive dryness of the skin may benefit from 12% ammonium lactate cream.
This condition more likely occurs in men with suboptimally controlled diabetes and who have obesity, use insulin and have other complications of their diabetes.
Please click on each section for more information
Skin changes happen slowly. Usual prognosis is:
- Thick, hard skin that feels smooth. You cannot pinch the skin over the upper back or neck. This condition is painless.
- Reddish, painless lesions.
- Lesions occur on the same areas on both sides of the body (symmetrical).
In severe cases, thickened skin can make it hard to move the upper body. It also can make deep breathing difficult.
Some people find it hard to make a clenched fist because the skin on the back of the hand is too tight.
There is no specific treatment for scleredema. Treatments may include:
- Improved control of glycaemia if needed (this may not improve the lesions once they have developed)
- Phototherapy, a procedure in which the skin is carefully exposed to ultraviolet light
- Glucocorticoid medications (topical or oral)
- Electron beam therapy (a type of radiation therapy)
- Medicines that suppress the immune system
- Physical therapy, if you find it hard to move your torso or breathe deeply
The condition cannot be cured. Treatment may improve movement and breathing.
- Find it hard to move your arms, shoulders, and torso, or hands
- Have trouble breathing deeply due to tight skin
- Keratosis Pilaris
Keratosis pilaris is a very common benign keratotic disorder. People with keratosis pilaris classically present with areas of keratotic perifollicular papules with surrounding erythema or hyperpigmentation. The posterior surfaces of the upper arms are often affected but involvement of the thighs, face, and buttocks can also be seen. Compared to the general population, keratosis pilaris occurs more frequently and with more extensive involvement of the skin in those with diabetes. Keratosis pilaris can be treated with various topical therapies, including salicylic acid, moisturizers, and emollients.

Many people without diabetes have skin tags, which are harmless growths that can appear anywhere on the skin. They are symptomatic of undiagnosed type 2 diabetes and insulin resistance. Studies have concluded that skin tags are an indicator for high cholesterol in people with type 2 diabetes and an increase in skin tags is indicative of type 2 diabetes.
Sometimes the tags are firmly fixed to the skin, some tags appear to dangle from a stalk. Skin tags can develop anywhere on the skin, but they are most common on the eyelids, neck, armpit, under breasts, around your bottom and groin. Skin tags range from 2mm – 5cm in size. They can appear on their own or a large group of them.


Images are from https://www.nhs.uk/conditions/skin-tags/

Image from https://www.ncbi.nlm.nih.gov/books/NBK481900/
They can be confused with warts or moles. They are considered cosmetic so will not be removed on the NHS.
–
Digital sclerosis
This condition starts with tight, thick, waxy skin on the fingers. It can cause finger joints to become stiff and hard to move. It can spread to other parts of the body, especially with elevated glycaemic levels. This condition is a long-term complication of suboptimally managed diabetes. There is no cure for digital sclerosis. It can occur in children and young people with type 1 diabetes
–
Diabetic Cheiroarthropathy

Positive Prayer sign (image from National Library of Medicine https://pmc.ncbi.nlm.nih.gov/articles/PMC9767792/)
Diabetic cheiroarthropathy or diabetic hand syndrome is one of the complications encountered in long-standing suboptimally controlled diabetes. It is characterized by limited movement of the joints of the hands along with thickening of the skin on the palmar and dorsal surfaces. There is an association between diabetic cheiroarthropathy and microvascular complications of diabetes, most commonly diabetic retinopathy. Early diagnosis of cheiroarthropathy can an opportunity to screen for microvascular complications. Cheiroarthropathy is usually a clinical diagnosis. Diabetic cheiroarthropathy can occur in long-standing diabetes. The prime pathophysiological mechanism includes formation of advanced glycation end products, cross linking of collagen and microangiopathy of blood vessels due to prolonged hyperglycaemia. This is a relatively common complication of long-standing diabetes mellitus. The majority of people also present with scleroderma-like skin changes,
There are no curative treatments. Symptomatic people may benefit from non-steroidal anti-inflammatory drugs or targeted injection of corticosteroids. This condition is best managed with regular stretching to maintain and minimize further limitations in joint mobility.
Treatment involves achievement of good glycaemic control along with physiotherapy and occupational therapy.
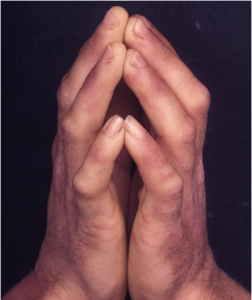
Image from https://www.ncbi.nlm.nih.gov/books/NBK481900/
–
Diabetic yellow skin and finger nails
Yellow discoloration can also be associated with hypothyroidism, liver disease and renal disease. It is common finding in people, especially older people with diabetes. Carotenemia is yellowish-red and can be found in some people with diabetes. It may also be associated with end-products of advancing glycation.

–
Mastopathy Eruptive Xanthomatosis
Eruptive xanthomas is a clinical presentation of hypertriglyceridemia, generally associated with serum triglycerides above 2,000 mg/dL (For adults, a normal triglyceride level is below 150 mg/dL. For young people between ages 10 and 19, a normal number for triglycerides is below 90 mg/dL). However, in people with diabetes, lower levels of triglycerides may be associated with this condition. The prevalence of Eruptive Xanthomatosis is around 1% in type 1 diabetes and 2% in type 2 diabetes. Serum lipid abnormalities are present in about 75% of people with diabetes.
Eruptive Xanthomatosis has been reported as the first presenting sign of diabetes mellitus, granting it can present at any time in the disease course. The condition presents as eruptions of clusters of glossy pink-to-yellow papules, ranging in diameter from 1 mm to 4 mm, overlying an erythematous area. The lesions can be found on extensor surfaces of the extremities, the buttocks, and in areas susceptible in injury. This condition is usually asymptomatic but may be pruritic or tender. The histology reveals a mixed inflammatory infiltrate of the dermis which includes triglyceride containing macrophages, also referred to as foam cells.
Lipoprotein lipase, a key enzyme in the metabolism of triglyceride rich lipoproteins, is stimulated by insulin. In an insulin deficient state, such as suboptimally managed diabetes, there is decreased lipoprotein lipase activity resulting in the accumulation of chylomicrons and other triglyceride rich lipoproteins. Increased levels of these substances are scavenged by macrophages . These lipid-laden macrophages then collect in the dermis of the skin where they can lead to eruptive xanthomas.
This condition can resolve with improved glycaemic control and a reduction in serum triglyceride levels. This may be achieved with fibrates or omega-3-fatty acids in addition to an appropriate insulin regimen.
–
Vitiligo

Vitiligo is an acquired autoimmune disorder involving melanocyte destruction. People with vitiligo present with scattered well-demarcated areas of depigmentation that can occur anywhere on the body, but frequently involves the acral surfaces and the face. Whereas about 1% of the general population is affected by vitiligo, vitiligo is much more prevalent in those with diabetes mellitus. Vitiligo occurs more frequently in women and is also more common in type 1 than in type 2 diabetes mellitus. Coinciding vitiligo and type 1 diabetes mellitus may be associated with endocrine autoimmune abnormalities of the gastric parietal cells, adrenal, or thyroid.


















