SCREEN NOW
Welcome to our educational section about SCREEN NOW
We hope this page and the resources within the page provide you with the information you need to learn more about diabetes and eye health and why diabetic retinal screening is so important
In this video Professor Anne Phillips and co-Chair of iDEAL Diabetes CIC introduces why screening for Diabetic Retinopathy and Macular Oedema for People with Diabetes is so important and discusses the value to the resources within this webpage regarding increasing knowledge and awareness of Diabetic retinal screening and early referral.
(Click the image below to play)
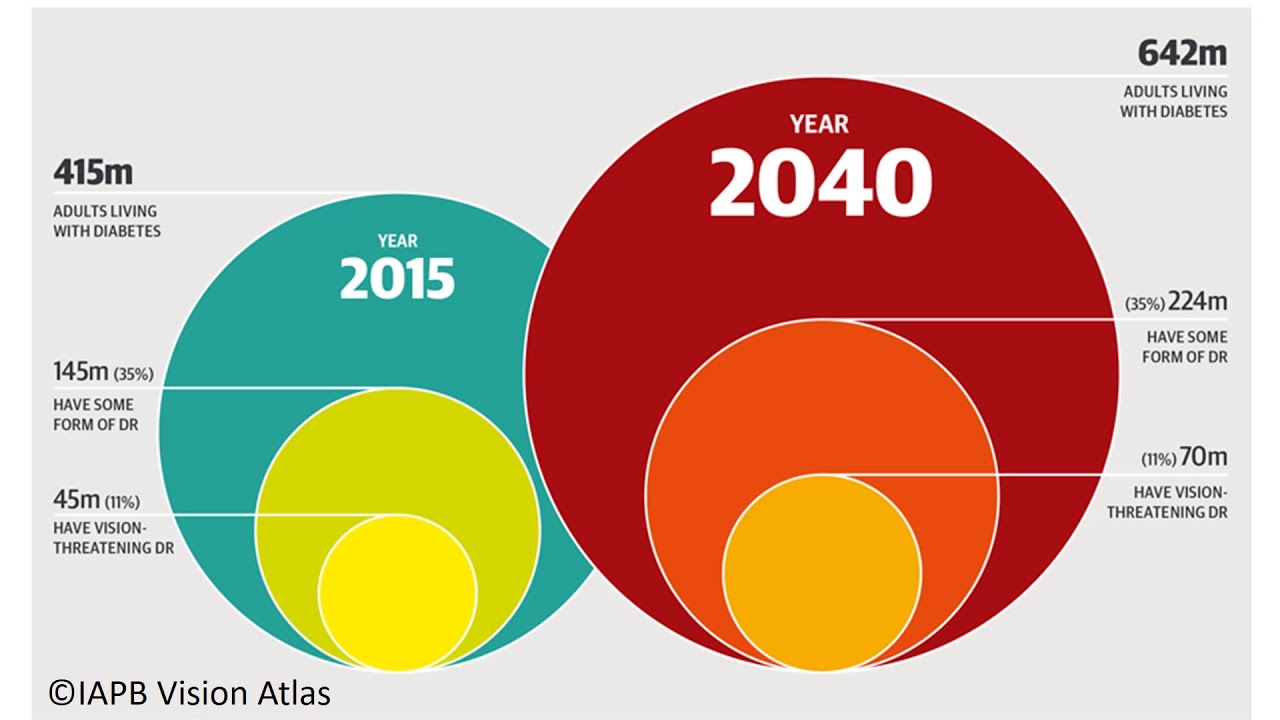
This map demonstrates the impact of Diabetic retinopathy globally and the predicted incidence by 2040 globally
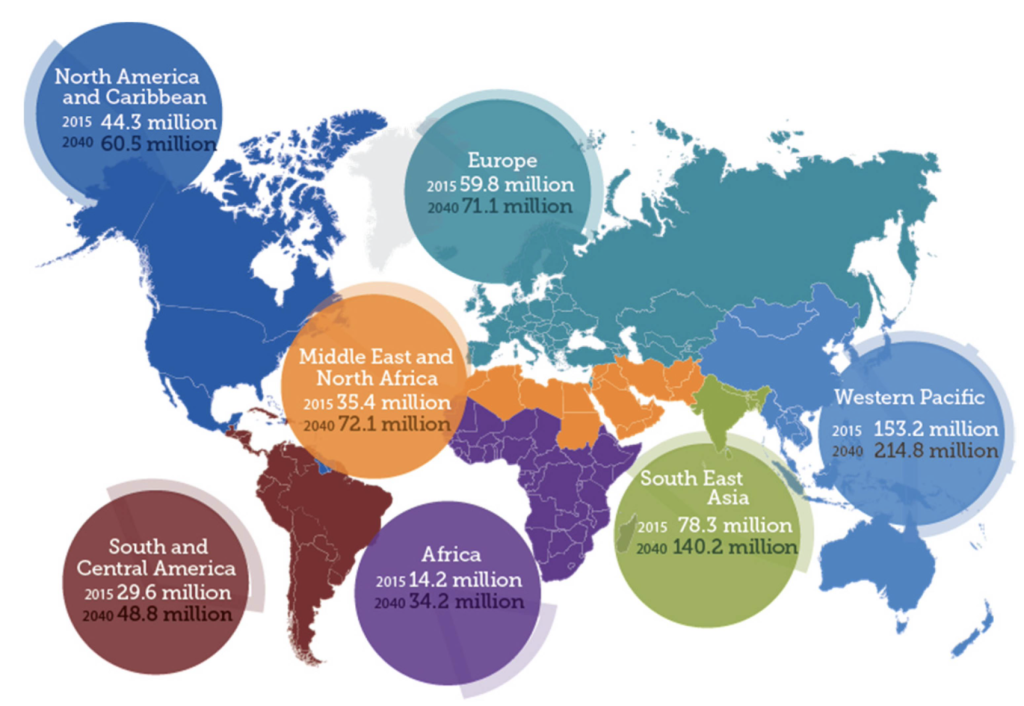
The International Agency for the Prevention of Blindness Vision Atlas demonstrates the impact and predicted incidence of Diabetic Retinopathy by 2040

Multi-disciplinary Health Care Professionals who work with People with diabetes at risk of or experiencing Diabetic Retinopathy and/or Macular Oedema
This animation which can be viewed below offers you the opportunity to promote SCREEN NOW and encourages its use with every person with diabetes
(Click the image below to play)
The UK National Screening Programme for Retinopathy which grades retinopathy is as follows:
| R – Number | Column 2 |
|---|---|
| R0 | No retinopathy present |
| R1 | Background Retinopathy present |
| R2 | Pre-proliferative retinopathy present |
| R3 | Proliferative retinopathy |
| M1 | Maculopathy |
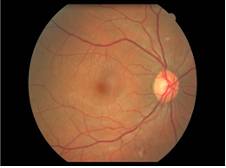
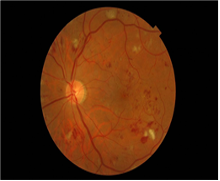
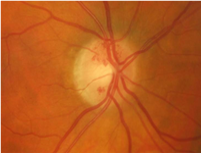
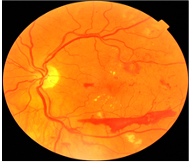
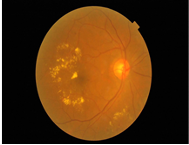
These images show how Retinopathy affects the eyes and how retinopathy is graded
R0 – no retinopathy present
R1 – Background retinopathy, showed here with cotton wool spots (CWS) and haemorrhages. This patient would continue with their annual check-ups, no treatment is needed at this stage.
R2 – Pre-proliferative retinopathy, CWS, Multiple deep, round or blot haemorrhages. This patient would be either referred into the hospital eye service or kept on close review by the diabetic eye screening service – 3 to 6 months review.
R3 NVD – Look at the appearance of the optic disc. These are classic looking NVD. New vessels appear messy in form, tangled and unstable. This patient would need urgent referral to the hospital eye service for anti-VEGF treatment with the added laser.
R3 NVE plus Pre-retinal bleed. The haemorrhage occurs from the unstable NVs bleeding into the internal limiting membrane. Same as the above treatment.
M1 Maculopathy –Characterised by the distribution of exudates, appearance is yellow waxy deposits of fat. This patient would be referred into the hospital eye service for anti-VEGF treatment
Diabetic Macular Oedema
Diabetic macular oedema (DMO) is the most common cause of sight loss in people with diabetes.
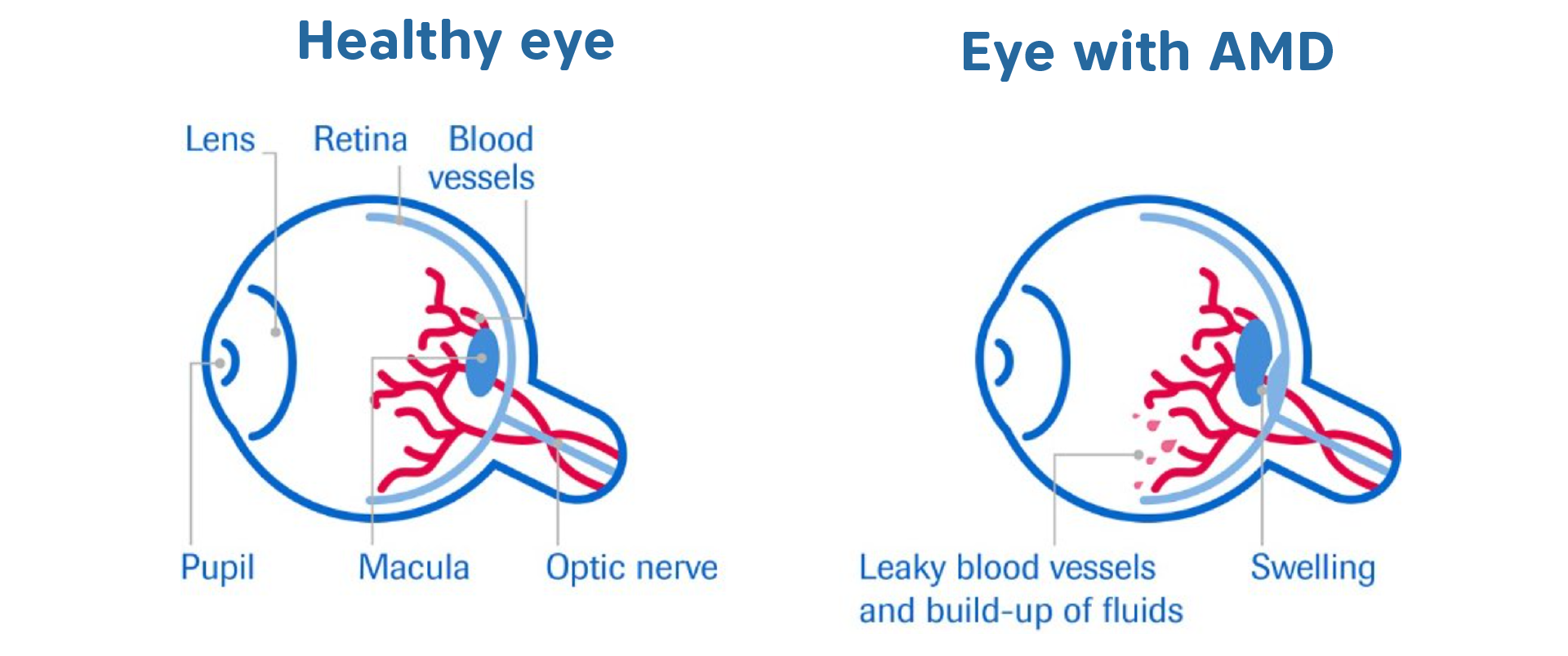
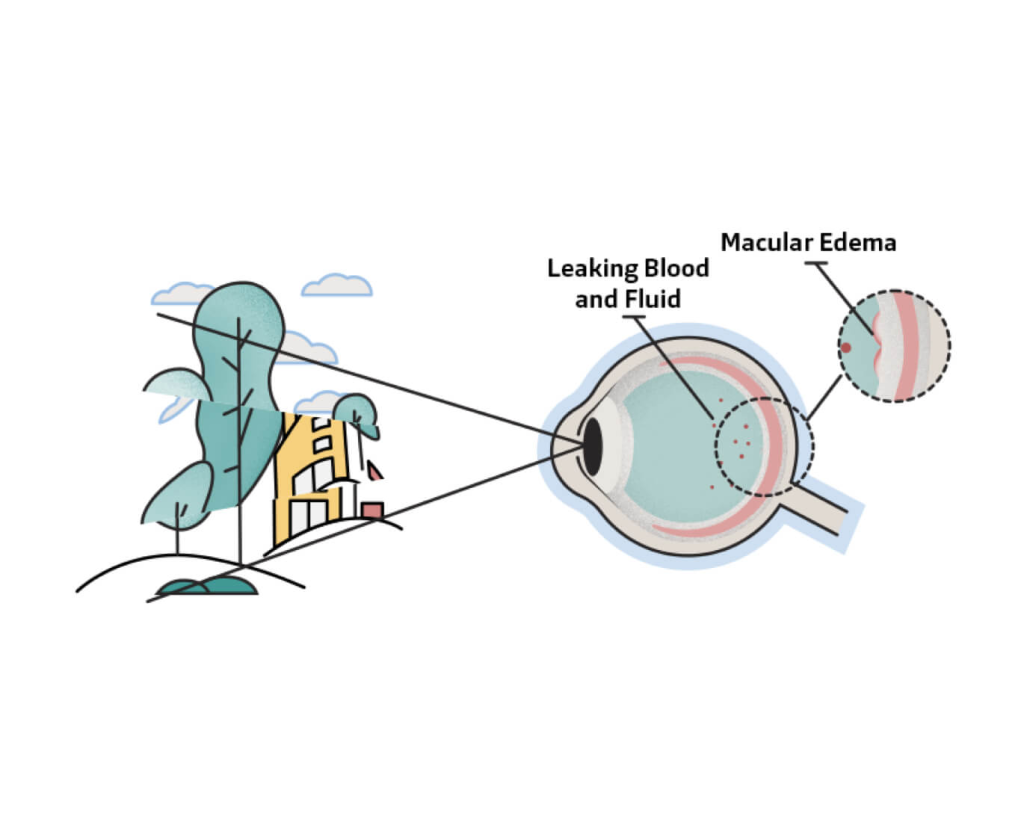
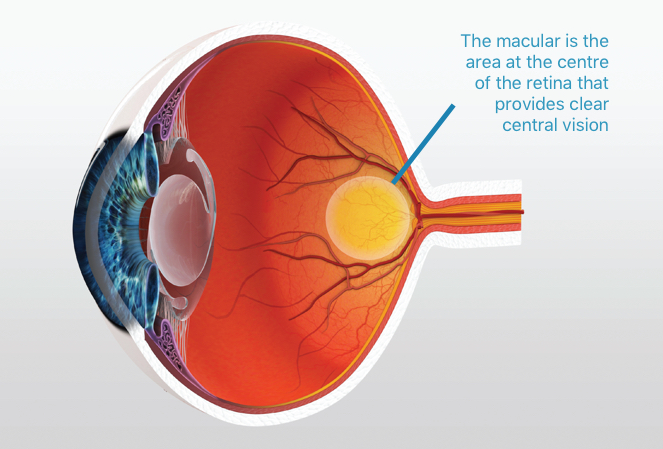
When leaky vessels cause fluid to build up in the macula, at the centre of the retina, it is known as diabetic macular oedema. It is a complication of diabetic retinopathy and results in a condition very similar to wet Age related Macular Degeneration (AMD).
Being diagnosed with diabetic macular oedema can be distressing and worrying but, with the right information and support, people can cope very well.
The condition is painless, and although macular oedema affects central vision, peripheral vision is not affected. However, other forms of diabetic retinopathy may affect your wider vision.
How diabetes affects your eyes
People with diabetes are at risk of damage to their eyesight. To work properly, the eye needs a constant supply of blood. When control of blood glucose and insulin levels in the body is suboptimal, the blood vessels of the eye can become damaged. The blood vessels of the retina are particularly prone to leaking and a condition known as diabetic retinopathy can develop.
People with diabetes can reduce their risk of vision loss by attending their annual diabetic eye screening appointment.
Symptoms
In the early stages of diabetes a person may not notice any effect on their vision. Damage to the retina occurs over many years.
It may affect the entire retina but when the damage causes only small bulges in the blood vessels of the retina, the eyesight remains good.
However, when the blood vessels in or close to the macula become damaged, or there is sudden bleeding or fluid leaking into the macula, then sight can worsen dramatically.
- Dark spots like a smudge on glasses or gaps may appear in your vision, especially first thing in the morning.
- Objects in front of you might change shape, size or colour or seem to move or disappear.
- Colours can fade.
- You may find bright light or glare difficult.
- You may experience difficulty reading.
- Straight lines such as door frames and lamp posts may appear distorted or bent.
If you notice a sudden change in your vision, contact your optometrist or hospital eye specialist urgently.
Risk factors
The longer you have diabetes, the greater your chance of developing sight loss through DMO. About 90% of people with type 1 diabetes may have some degree of retinopathy after 10 years.
For people with type 2 diabetes the chance of developing some degree of retinopathy after 10 years varies between 67–80% (or two in three to four in five), depending on whether they need to take insulin.
More than a third of all people with diabetes will develop a level of severity of macular oedema which, without changes to the person’s lifestyle and better control of blood glucose, will require treatment.
If you have high blood pressure as well, you have a higher risk of developing advanced retinopathy. Overall, 7 per cent (around one in 14) of all people with diabetes develop DMO, which will result in a noticeable loss of vision.
Diagnosis
If DMO is suspected, you will be referred to the eye hospital for tests. Your hospital specialist (ophthalmologist) may use:
- Eye drops to dilate the pupils to allow them to clearly see the back of the eye. The drops may make your vision blurred and sensitive to light for a short time so consider taking someone with you.
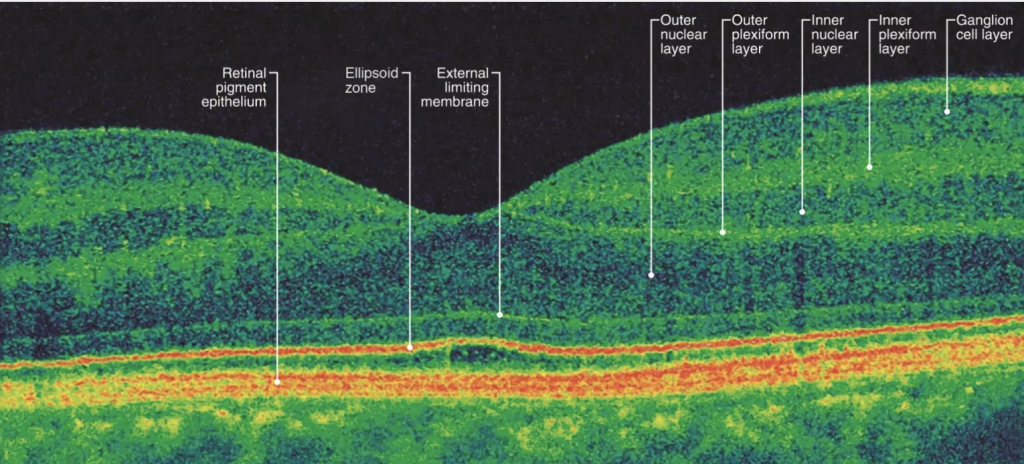
- Scans using optical coherence tomography (OCT) to produce a cross-sectional image of the retina. (See images below)
- Fluorescein dye angiography. A dye is injected into a vein in the arm. It travels to the eye, highlighting the blood vessels in the retina so they can be photographed. The dye will temporarily change the colour of your urine.
If you have any vision problems in between your appointments seek immediate advice from your diabetes care team or GP. Do not wait until your next hospital appointment.
Treating DMO
DMO can be treated if caught early. Drugs are injected into the eye to stop fluid leaking from the blood vessels. Following diagnosis, people will usually have a number of injection treatments in the first few months. Subsequent check-ups will then be required to assess when more injections are needed.
The injections are not as bad as they might sound. The eye is anaesthetised and the needle goes into the corner of the eye so the patient does not see it. These are called intravitreal injections. The treatment cannot restore sight if there is already significant damage to the macula.
There are drugs in use for treating DMO: They act on the blood vessels in the retina to reduce fluid leakage that leads to oedema in the eye.
The frequency and number of injections depends on how a patient responds to the drug. Ask your eye doctor about your treatment programme. Do not miss a treatment session – any sight loss cannot be recovered.
Anti-VEGF treatment
Anti-VEGF treatments are a group of medicines which reduce new blood vessel growth (neovascularisation) or oedema (swelling).
Anti-VEGF medicines can be used to treat a number of eye conditions that cause new blood vessel growth or swelling under the macular area of your retina, the lining of the back of (the eye.)
The macula is a tiny area of your central retina, which is very important for seeing detail, colour, and objects directly in front of you. When there is new, abnormal blood vessel growth or swelling at the macula, it can cause problems with your central detailed vision and with tasks such as reading, watching television, or recognising faces. Anti-VEGF treatment usually must be started quickly before the new blood vessels or swelling does too much damage to the macula.
How is anti-VEGF treatment given?
Anti-VEGF treatment is given as an injection into the white of your eye (the sclera). The drug is injected directly into the vitreous, the jelly that fills your eye. This is called an “intravitreal” injection. The procedure is generally very straightforward and quick and isn’t usually painful.
This video from the Royal National Institute for the Blind demonstrates a gentleman call Reg talking about having his anti-VEGF injections.
Laser treatment
Some people may be offered laser treatment when the DMO does not involve the centre of the macula. This treatment aims to stabilise vision and does not generally improve sight. It usually involves one or more visits to an outpatient laser clinic for treatment by an ophthalmologist.
Before the procedure, local anaesthetic will be administered to the surface of your eye, as well as eye drops to widen your pupils. A special contact lens will be placed on your eye to hold your eyelids open and allow the laser beam to be focused onto your retina. Laser treatment is not usually painful, but you may feel a sharp pricking sensation.
Protecting your eyes
Diabetes is a lifelong condition, so maintaining a healthy lifestyle and monitoring your blood glucose, blood pressure and cholesterol levels is crucial to avoid damage to your eyes.
It is essential that you attend your diabetes clinic appointments. Your diabetes care team will maintain and monitor your diabetes care plan. Make sure that your eyes are screened at least once a year to spot any problems early.
If you wear glasses or contact lenses continue to visit your optician regularly.
Devices for people with Diabetes who are partially sighted or blind to use
Blood Glucose Monitoring Devices
The Prodigy Voice® talking glucose meter is a totally audible blood glucose monitoring system specially designed for the blind. The features were developed with the help of National Blind Associations and Certified Diabetes Educators.
Continuous Glucose Monitoring
Dexcom G6 with Apple Siri feature is the first and only real-time CGM that can be used by visually impaired patients to access their glucose levels.
Insulin injections
A visual magnifying window can help people who are visually impaired to see the correct doses to inject
Insulin pens that also click the dial up does can help people visually impaired to maintain their independence
Insulin pumps that beep, have audible tones and vibrations are in development for people with diabetes and visual impairment
This link takes you to how to manage prescription medications if visually impaired or blind: (https://www.wikihow.com/Organize-Your-Medications-if-You%27re-Blind-or-Visually-Impaired)
These are some devices for people who are partially sighted or blind to use
Voice activated phone use can help people who are visually impaired


Using tech vocally can help people with visual impairment or blindness to remain employed and able to continue to use such technologies
Enlarged text can help people with visually impairment


Hi Siri can assist around the individuals home environment
Talking Books are useful for people with visual impairment or blindness

Other visual aids which magnify images can offer assistance
This SCREEN NOW Project Webpage and contents has been created by an independent Multi-Disciplinary Team. Viatris provided sponsorship for the development and production of this webpage but has had no input into the content